Consultation
Regardless of whether you are seeking medical advice for the first time, or your gynecologist or urologist has already determined that you need fertility therapy, you are welcome to make an appointment at our practice – preferably together with your partner. Please bring any previous test results with you. You may not need any new examinations. After one year of regular sexual intercourse without contraception, pregnancy occurs in about 85% of all couples. There can be many reasons why it has not yet worked for you. The most common reasons include cycle disturbances, damage to the fallopian tubes or limited sperm quality.
During an initial consultation with you, we first discuss your „history“. Is your cycle regular? Have you already had infertility treatments? The completed
questionnaires, which you will have access to once you make your appointment, also contain helpful information for us. We can then arrange the necessary diagnostic measures depending on how long you have been trying to get pregnant. It is however not always possible to find a reason for the absence of pregnancy and this is called idiopathic infertility. Often an initial recommendation can be given at the end of the consultation. Sometimes we also arrange a further consultation. It is important to us that you are able to ask all your questions and address all your concerns during the consultation. Ultimately, you decide whether and when a particular therapy will be carried out.
Laboratory tests
The hormonal balance in the body is a delicate interplay between many parameters. Thus, various hormonal disorders can be the cause of a woman not becoming pregnant or having repeated miscarriages. A blood test can detect malfunctions of the thyroid gland, the pituitary gland (e.g. elevated prolactin levels) or even the adrenal cortex and ovaries (e.g. elevated male hormones). The hormones of the ovary (estradiol, corpus luteum hormone) change during the cycle and are therefore determined at various time points, often multiple times during a cycle.
Some general hormonal disorders are common, for example hypothyroidism, elevated prolactin levels (hyperprolactinemia) or diabetes mellitus including its
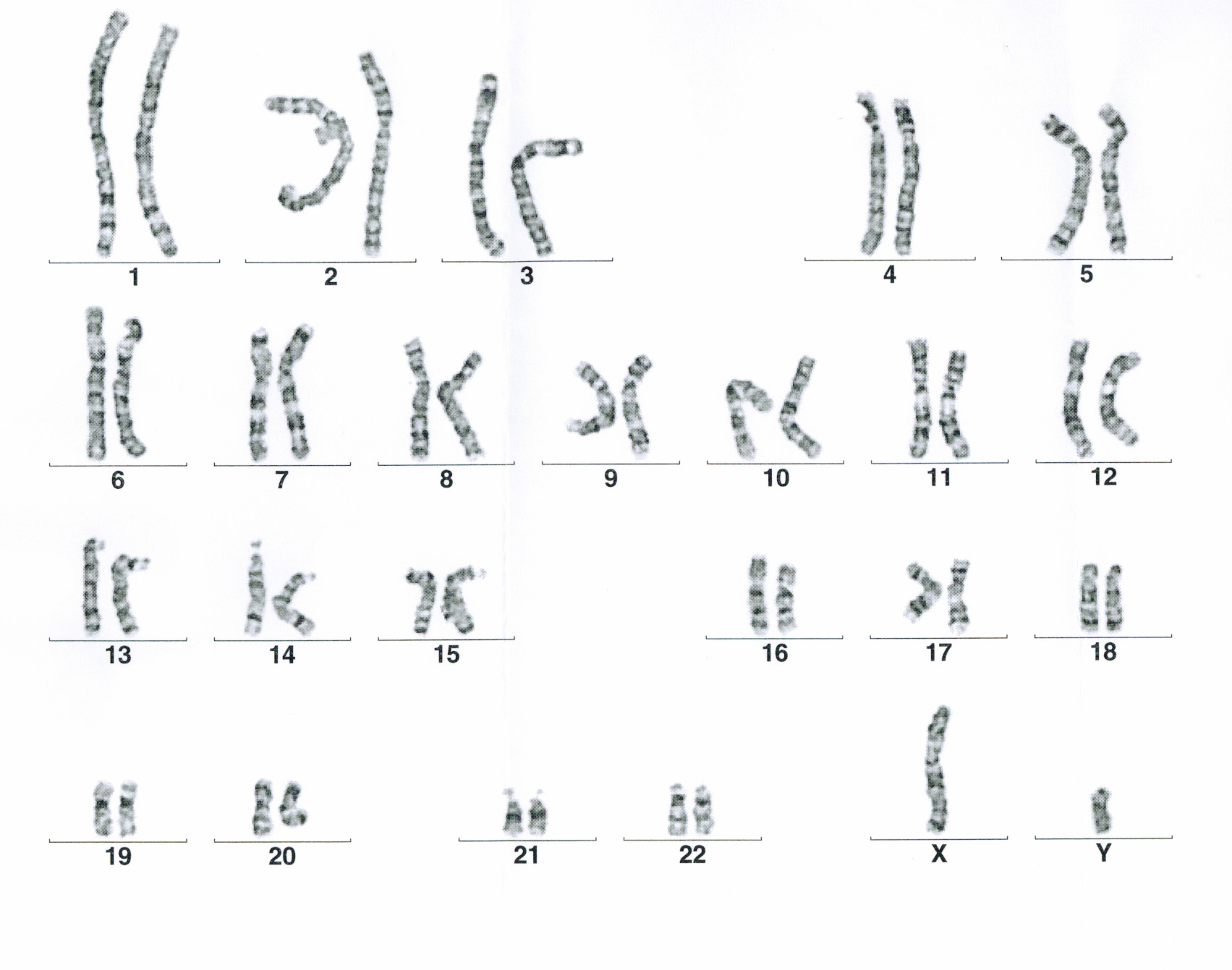
precursor. These should be properly controlled with medication before the start of targeted gynecological treatment. We offten apply strcter criteria to infertility patients than perhaps your family doctor or internist. If this alone is not sufficient, hormone stimulation can be carried out, i.e. egg maturation, ovulation and support oft he corpus luteum phase. Before fertility treatment, serological tests for HIV, hepatitis B and C are necessary in both partners. Chromosomal analysis from a blood sample in both the man and woman is recommended prior to ICSI therapy and for diagnosis in cases of repeated miscarriages. These blood samples can of course also be taken in our practice.
Sperm Assessment
We are aware that sperm collection in a medical setting is uncomfortable for many men. We do our best to try to make the situation easier for you and practice the utmost discretion. There are two separate sperm collection rooms in our practice. When you have a spermiogram appointment, one of our laboratory staff will take you to the donor room where you will be given a sterile cup with your name on it and can ask any questions you may have. In the donor room, which can be locked from the inside, you will have plenty of time to provide a sample. Relevant videos are available to you, and your partner can of course accompany you.
The evaluation for a spermiogram takes some time, so there is no need to wait in the practice. The result will be sent to you by mail, or you can request it by
phone. Before a spermiogram, sexual abstinence should be observed for three to five days. If sperm collection at the clinic is not an option for you, it is also possible to collect the ejaculate at home and transport it to the clinic, keeping it warm, for examination. The examination is carried out immediately upon receipt of the sample in our laboratory. The number (concentration), motility (movement) and shape (morphology) of the sperm are assessed under a microscope. If an infection is suspected, a bacterological examination can be arranged. The spermiogram findings are decisive for our therapy recommendation, however a man’s spermiograms are subject to certain fluctuations, and a follow up test is often recommended in the case of initial abnormal results.

Important information to our Spermiogramm
| Normal values of sperm | |
|---|---|
| Normozoosperm | normal ejaculate parameters |
| Oligozoosperm | reduced concentration of sperm |
| Asthenozoosperm | reduced mobility of sperm |
| Teratozoosperm | reduced morphology of sperm |
| Oligoasthenoteratozoosperm (OAT) | reduced concentration, mobility and morphology |
| Azoosperm | no sperm in the ejaculate |
| WHO 2021 normal values of sperm | |
| Concentration (number of sperms) | >= 15 millions/ml or total number of sperms >= 39 Mio. |
| Progressive mobile sperm (categories A+B) | >=30 % |
| Local and immobile sperm (categories A+B+C) | >=42% |
| Morphology (Sperm form, different guidelines here) |
4% |
DNA Fragmentation Test
A variety of factors can lead to strand breaks (fragmentations) in the DNA of sperm. With the help of the DNA fragmentation test (halosperm test), your sperm can be examined for DNA damage by using a special staining method. During the procedure, the sperm are treated and stained so that the chromosomal DNA unfolds and wraps around the sperm head in the form of loops (a halo). In sperm with fragmented, i.e. broken DNA, these loops do not form or only form very
weakly. Therefore, no halo is seen.
The most important factor to be taken into account from this test, is the „DNA Fragmentation Index“ (DFI). The higher this index, the lower the probability of natural fertilization and thus pregnancy and birth. The result provides the doctor detailed information about sperm quality, and supports selection of the appropriate treatment method (insemination, IVF or ICSI).
Menstrual cycle monitoring
The purpose of cycle monitoring is to determine whether you have an ovarian follicle, ovulation and corpus luteum formation. Normally, an egg cell grows in the follicle every month. After ovulation, the egg cell enters the fallopian tube and is fertilised by a sperm. Only four days later does the fertilised egg arrive in the uterus and implant in the uterine lining. During the first weeks of pregnancy, the corpus luteum, which is formed on the ovary from the ruptured follicle, produces the hormone progesterone to support pregnancy. Women with regular, approximately 28-day cycles, are generally expected to have unremarkable cycles when monitored. Women who have a prolonged cycle, irregular bleeding or the first signs of menopause, should have their follicle growth checked if they wish to have children.
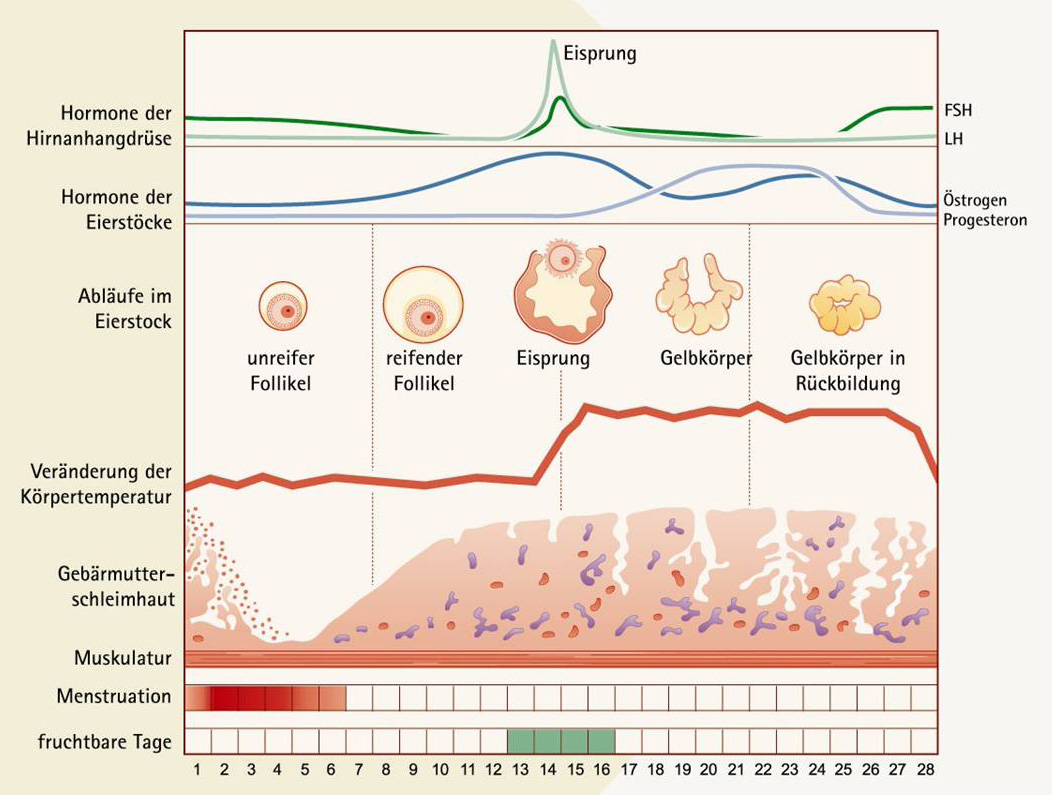
For this purpose, an ultrasound examination (vaginal) is performed on the 10th cycle day. The follicles on the right and left ovaries and the thickness oft he endometrium are measured. Usually, only one larger follicle is seen. If this is not yet large enough, it is checked again after two days. A ripe follicle measures about 20mm. Often a number of smaller follicles (around 10mm) can be seen at the same time. If a larger follicle is present, a blood sample is taken to determine E2 (estradiol) and LH (Luteinizing hormone). The estradiol correlates with the maturity of the egg and the LH surge causes ovulation. An optimal case would be the detection of an 18-22mm follicle at mid-cycle with adequate estradiol and LH levels. There are variations from cycle to cycle, however if you have no follicle growth over multiple cycles, we will recommend hormone stimulation.

Fallopian Tube Patency
There are different methods used to check the patency of the fallopian tubes. One option is a laparoscopy with tubal patency testing (chromopertubation). With the help of a catheter, coloured fluid is injected via the uterus into the fallopian tubes, which then passes into the free abdominal cavity, and can be observed directly with a camera during the laparoscopy. The procedure is performed under general anasthesia, but usually on an outpatient basis, which means that you can leave the clinic again on the same day. This method provides the most reliable information about the condition oft he fallopian tubes and is especially recommended for patients with previous operations or after abdominal

Es gibt verschiedene Methoden, die Durchgängigkeit der Eileiter zu prüfen. Eine Möglichkeit ist eine Bauchspiegelung mit Eileiterdurchgängigkeitsprüfung (Chromopertubation). Mit Hilfe eines Katheters wird farbige Flüssigkeit durch die Gebärmutter in die Eileiter gespritzt, die anschließend in die freie Bauchhöhle
inflammation.
The least invasive method (also without anasthesia) to check tubal patency is by sonography (ultrasound). Since the fallopian tubes cannot normally be visualized by sonography, a harmless solution (foam ExEm® Foam Kit) is introduced into the uterus via a small plastic catheter. This foam produces a quick and easy expansion of the fallopian tube walls, which can be seen on the ultrasound image. This examination is performed in our practice and is particularly suitable for patients without previous gynecological disease.

Hysteroscopy
For a hysteroscopy, a long, approximately 3mm thin camera instrument (hysteroscope) is inserted into the uterine cavity, and saline solution is flushed through this, so that the uterine cavity unfolds.
The interior of the uterus with the opening to the fallopian tubes can then be seen on the monitor and abnormalities can be detected. The examination takes a
few minutes and is performed in the first half of the menstrual cycle. It is offered in our practice (with or without anesthesia).
Malformations of the uterus that exist since birth (for example a septum in the uterus) can be removed surgically. Also fibroids and cluttering of the endometrium can interfere with pregnancy and would need to be removed before starting therapy.
Special diagnostics for repeated miscarriages or implantation failures
Miscarriages occur in 11-15% of all pregnancies. The percentage will increase continuously with women´s age reaching 50% once the women´s are past age 45. The reason for this are randomly occurring chromosomal defects, which can not be treated. However, if there are 3 or more consecutive miscarriages it is referred to as abitual abortions. This concerns 1% of all pregnancies. In some of the patients defects can be defected that can be treated, so further examinations may be useful.
- Hysteroscopy – to exclude malformations of the uterus
- Blood sample for chromosomal analysis – to exclude congenital genetic defects
- Blood sample for hormone analysis -to exclude hormonal causes (eg thyroid gland malfunction)
- Blood sample to exlude imbalance of clotting factors and antibodies as a cause
- Biopsy of the endometrium (the lining of the uterus) for immunohistological examination for uterine killer cells or plasma cells as a sign of inflammation
In some patients with recurrent miscarriage or implantation failure, treatable disorders can be diagnosed. A biopsy of the endometirum (the lining of the
uterus) may be taken for immunohistological examination for uterine killer cells or plasma cells, which can be a sign of inflammation.

