ICSI Therapie
/in ICSI (Intracytoplasmatische Spermieninjektion)/by econsorDie ICSI (Intrazytoplasmatische Spermieninjektion) ist eine spezielle Methode der In-vitro-Fertilisation. Sie wird eingesetzt, wenn eine schwere Störung der Spermienqualität vorliegt (siehe Spermientest). In diesem Fall geht man davon aus, dass die Spermien nicht in der Lage sind, aus eigener Kraft in die Eizelle einzudringen. Bei der herkömmlichen IVF-Behandlung, bei der Eizellen und Spermien lediglich in einer Kulturschale zusammengebracht werden, käme es daher nicht zu einer Befruchtung. Bei der ICSI-Therapie wird daher in jede reife Eizelle ein einzelnes Spermium des Partners injiziert. Dazu wird die Eizelle unter ein Mikroskop gelegt, mit einer Glaskapillare angesaugt und festgehalten. Anschließend wird ein gut bewegliches Spermium durch eine zweite dünne Glaskapillare hochgezogen und direkt in die Eizelle eingebracht. ICSI ist also ein zusätzliches Verfahren im Labor, aber für die Patientin sind die Behandlungsschritte identisch mit der IVF-Therapie.
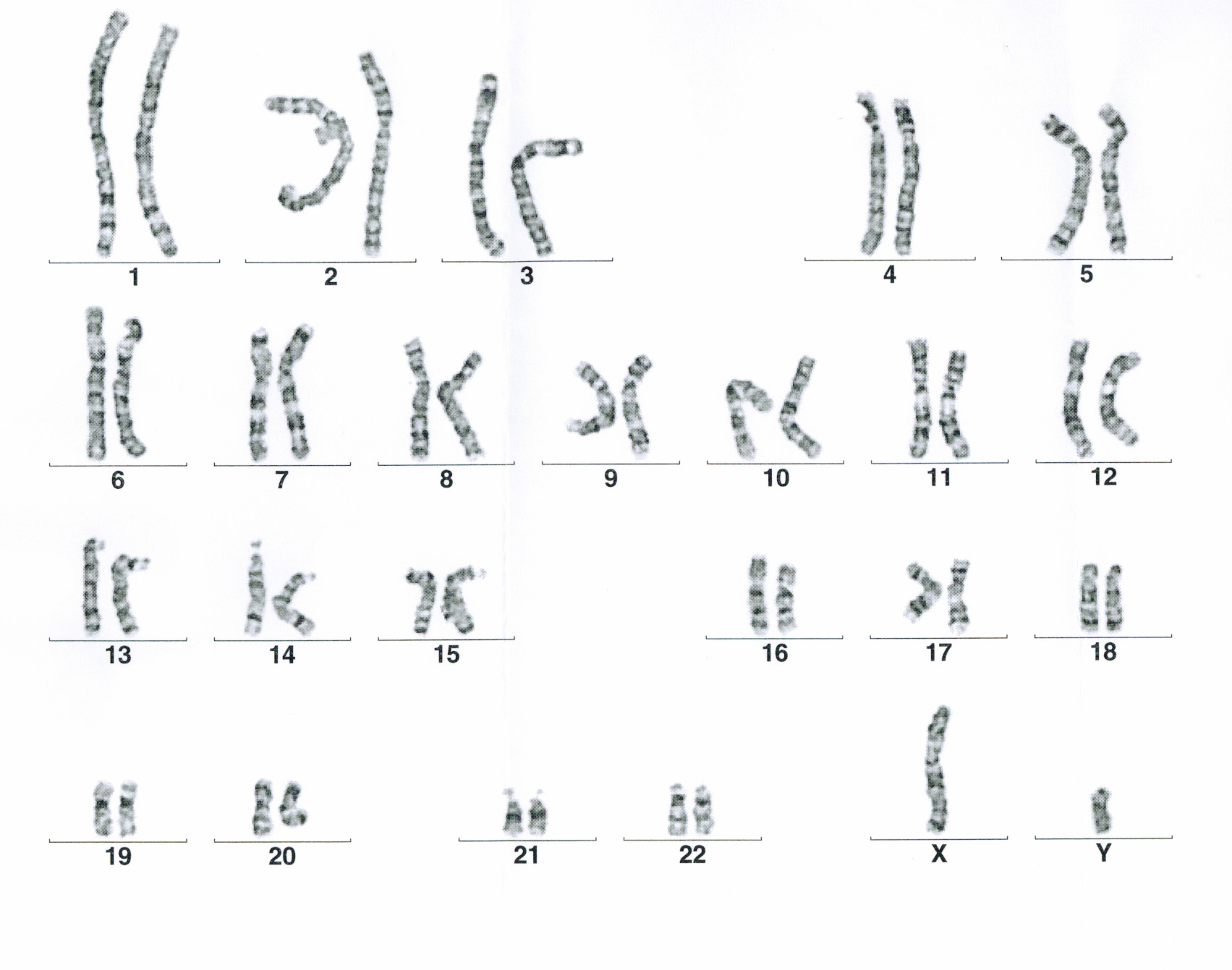
Vor Beginn der Therapie muss geklärt werden, ob eine konventionelle IVF oder eine ICSI notwendig ist. Der entsprechende Antrag auf Kostenübernahme kann bei Ihrer Krankenkasse gestellt werden. Diesen Antrag erhalten Sie von uns, nachdem wir Ihnen in einem Beratungsgespräch die Kosten- und Versicherungssituation erläutert haben. Für die ICSI-Therapie sind zwei Spermiogramme im Abstand von 12 Wochen erforderlich, die den Kriterien der Krankenkassen entsprechen. Es kann daher sein, dass nach dem Erstgespräch ein weiteres Spermiogramm erforderlich ist. Zusätzlich wird eine Chromosomenanalyse bei beiden Partnern empfohlen. In den neuen Richtlinien zur künstlichen Befruchtung 2017 ist festgelegt, dass Männer vor einer ICSI-Therapie von einem andrologisch qualifizierten Arzt untersucht werden müssen.